Electronic Medical Records (EMR) vs. Electronic Health Records (EHR): A Comprehensive Comparison of Systems
Introduction
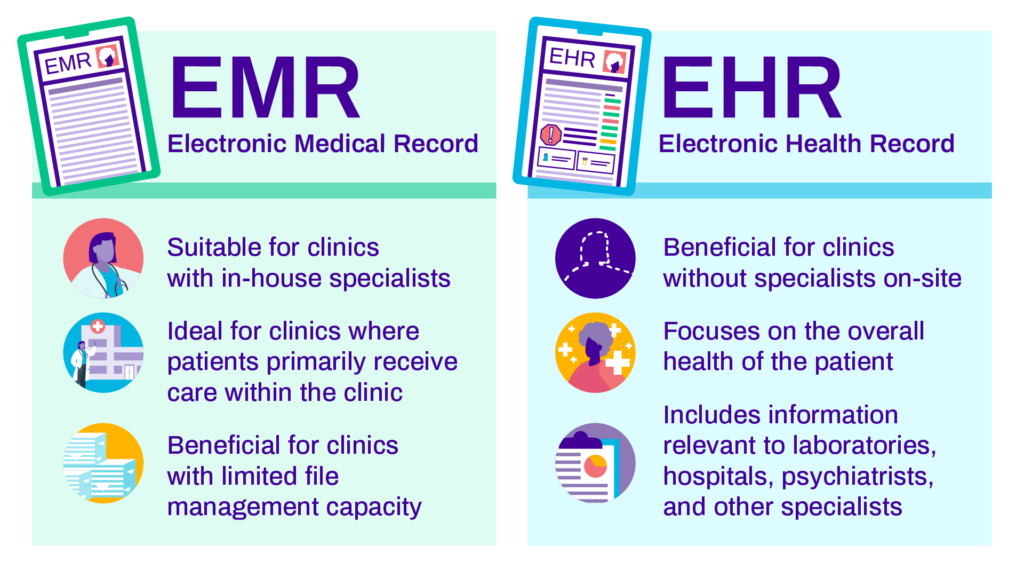
The digital revolution has transformed the healthcare industry, replacing traditional paper-based patient records with electronic systems. Two primary electronic systems in use today are Electronic Medical Records (EMR) and Electronic Health Records (EHR). These systems have streamlined patient data management and improved patient care, but they differ in scope and functionality. In this article, we will delve into the world of EMR and EHR, highlighting the pros and cons of each system, while also emphasizing the importance of maintaining the integrity of healthcare data and avoiding plagiarism in the context of medical records.
- Understanding EMR (Electronic Medical Records)
Pros:
a. Focused Patient Data:
EMRs are designed to store and manage patient-specific medical data. They provide a comprehensive view of a patient’s medical history, including diagnoses, treatments, and lab results.
b. Specialized Use:
EMRs are typically used by individual healthcare facilities or practices. This specialization allows for tailored features that meet the specific needs of the practice, making them efficient for smaller healthcare providers.
c. Enhanced Workflow:
EMRs can improve workflow within a healthcare facility by reducing paperwork, automating data entry, and facilitating quick access to patient information.
Cons:
a. Limited Data Sharing:
EMRs are often not interoperable, meaning they may not easily share data with other healthcare facilities or systems. This can hinder coordinated care, especially in cases of patient referrals or emergencies.
b. Narrower Scope:
EMRs focus primarily on clinical data and may not include a broader view of a patient’s health, such as lifestyle or social determinants of health.
c. Potential Data Isolation:
In larger healthcare systems or networks, different departments or specialties may use separate EMR systems, leading to data isolation and fragmented patient records.
- Exploring EHR (Electronic Health Records)
Pros:
a. Comprehensive Health Record:
EHRs encompass a broader range of health-related information, including clinical data, medical history, medication lists, allergies, immunizations, and even lifestyle factors. This provides a more holistic view of a patient’s health.
b. Data Interoperability:
EHRs are designed for data sharing and interoperability, enabling healthcare providers to access patient records from different facilities, improving care coordination.
c. Patient Engagement:
EHRs often have patient portals that allow individuals to access their health records, communicate with healthcare providers, and actively engage in their care.
Cons:
a. Complexity:
The comprehensive nature of EHRs can make them more complex to implement and navigate. Training and system integration can be challenging.
b. Cost:
EHR systems can be expensive to implement and maintain, especially for smaller healthcare practices. The initial investment and ongoing maintenance costs can strain budgets.
c. Data Security and Privacy:
With increased data sharing and accessibility, there are heightened concerns about data security and patient privacy breaches. Safeguarding patient information is paramount.
- The Importance of Data Integrity and Avoiding Plagiarism
In healthcare, data integrity is fundamental. Accurate, complete, and reliable patient records are crucial for providing high-quality care and ensuring patient safety. Plagiarism in the context of medical records can have severe consequences, including misdiagnosis, mistreatment, and compromised patient trust.
Here’s how to maintain data integrity and avoid plagiarism:
a. Accurate Data Entry:
Ensure that all patient data is accurately recorded and entered into the system. Any errors or inaccuracies can lead to serious medical mistakes.
b. Source Attribution:
When importing data from external sources or referencing other medical records, proper source attribution is essential. Always credit the source of information.
c. Data Verification:
Cross-verify information whenever possible, especially when dealing with critical patient data. This can help identify discrepancies or errors.
d. Data Security:
Implement robust data security measures to protect patient records from unauthorized access, breaches, or data theft. Comply with HIPAA regulations.
e. Ethical Data Use:
Use patient data ethically and responsibly. Avoid using patient information for any purpose other than providing healthcare or for research purposes with proper consent.
f. Regular Audits:
Conduct regular audits of patient records to identify any anomalies or irregularities. This can help maintain data accuracy.
- The Future of Healthcare Data Management
The healthcare industry is continually evolving, with an increasing emphasis on data sharing, patient engagement, and interoperability. The adoption of Health Information Exchanges (HIEs) and Health Information Portability and Accountability Act (HIPAA) regulations has catalyzed this transformation. Healthcare providers are now more accountable than ever for the security and integrity of patient records.
a. Interoperability:
The demand for interoperable systems is driving the development of more advanced EHR solutions. Seamless data sharing among healthcare facilities and systems is becoming the norm.
b. Patient-Centric Care:
Patient engagement and patient-centered care are central to modern healthcare. EHRs will continue to evolve to accommodate greater patient involvement in their healthcare journey.
c. Data Analytics:
Advanced analytics and Artificial Intelligence (AI) are increasingly being used to derive insights from healthcare data, aiding in diagnosis, treatment, and preventive care.
d. Telehealth:
The COVID-19 pandemic accelerated the adoption of telehealth services. EHRs are integrating telehealth features to facilitate remote consultations and care.
Conclusion
EMRs and EHRs have revolutionized healthcare data management, offering distinct advantages and challenges. The choice between the two systems depends on the specific needs of healthcare providers and the scale of operations. However, regardless of the system in use, the integrity of patient data and ethical practices must remain paramount. Plagiarism or inaccuracies in medical records can have dire consequences, jeopardizing patient safety and trust. As the healthcare landscape continues to evolve, healthcare providers must remain vigilant in upholding the highest standards of data integrity, security, and ethical data use. The future of healthcare data management holds promise, but it also brings greater responsibility in safeguarding patient information and ensuring the highest quality of care.


